When it comes to sexually transmitted infections (STIs), many are familiar with conditions like chlamydia, gonorrhea, or syphilis. However, there’s a lesser-known STI that’s increasingly becoming a health concern — Mycoplasma genitalium, often referred to as Mgen. While not as widely discussed as other STIs, Mgen is now recognised as a significant cause of genital infections, leading to uncomfortable symptoms that can be mistaken for other conditions. This blog will delve into what mycoplasma genitalium is, how it affects the body, and the best ways to manage it.
1. What is Mycoplasma Genitalium?
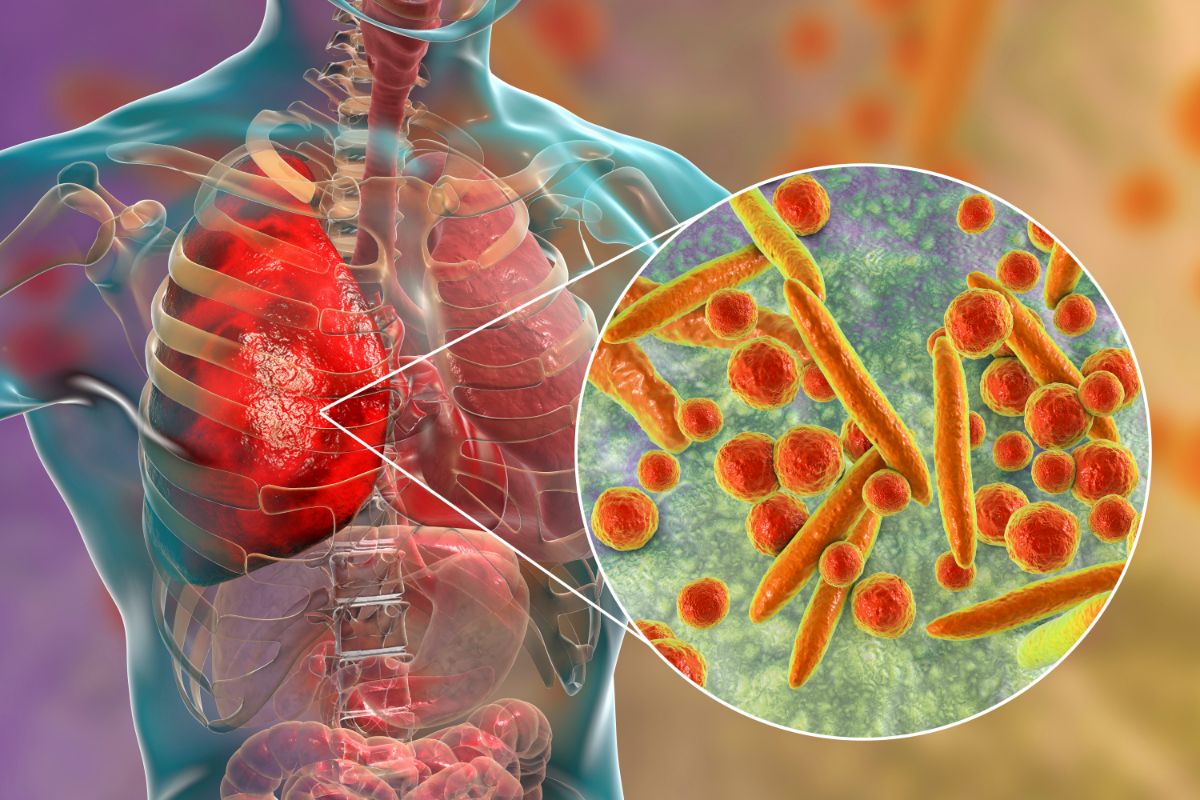
Mycoplasma genitalium is a sexually transmitted bacterium that affects both men and women. Discovered in the 1980s, it has gained more attention recently due to its role in genital infections and its ability to be resistant to certain antibiotics. Unlike many other STIs, Mgen doesn’t always produce immediate or obvious symptoms, which can make it challenging to diagnose.
The bacterium lives in the mucous membranes of the urinary and genital tracts. Its primary transmission method is through unprotected sexual contact, including vaginal, anal, and oral sex. As with other STIs, safe sexual practices can greatly reduce the risk of infection, but understanding this infection and its implications is key to prevention.
2. Common Mycoplasma Genitalium Symptoms
One of the main reasons Mycoplasma genitalium often goes undetected is its ability to remain asymptomatic for long periods. However, when Mgen symptoms do appear, they can closely resemble those of other common STIs, making it difficult to pinpoint the exact cause without proper testing. The following are some of the typical mycoplasma genitalium symptoms you may experience:
Symptoms in Women:
- Pain during intercourse (dyspareunia): One of the hallmark symptoms in women is discomfort or pain during sexual activity. This can sometimes be misinterpreted as a result of another condition, but Mgen may be to blame.
- Vaginal bleeding after sex: Unusual bleeding, especially after intercourse, may be another sign of infection.
- Unusual vaginal discharge: Infected women may notice changes in their vaginal discharge, including abnormal color, texture, or odor.
- Pelvic pain: Persistent lower abdominal pain can also indicate a Mycoplasma genitalium infection.
- Burning sensation during urination: If you experience discomfort or a burning feeling while urinating, this could be a symptom of Mgen.
Symptoms in Men:
- Urethritis: Inflammation of the urethra is common in men, causing painful or frequent urination.
- Discharge from the penis: Clear or cloudy discharge from the penis can also signal a Mycoplasma genitalium infection.
- Pain in the testicles: Men may experience discomfort in the testicles, which could be linked to infection.
- Discomfort during urination: A burning or stinging sensation during urination is another common Mgen symptom.
It’s important to note that some people may carry Mgen without ever experiencing symptoms. This asymptomatic nature of the infection means that many may unknowingly pass it on to their sexual partners, which is why regular STI screenings are critical.
3. How is Mycoplasma Genitalium Diagnosed?
Diagnosing Mycoplasma genitalium can be tricky due to its non-specific symptoms and the fact that it’s often mistaken for other STIs like chlamydia or gonorrhea. Testing for Mgen isn’t as widely available as testing for more well-known STIs, but it is crucial to get a correct diagnosis to ensure proper treatment.
Here are some steps typically involved in diagnosing Mycoplasma genitalium:
- Medical History and Symptom Review: Your doctor will review your sexual history and ask about any symptoms you’re experiencing. It’s important to be open and honest to receive the best care possible.
- Nucleic Acid Amplification Test (NAAT): This is the gold standard for diagnosing Mgen. The test detects the DNA of the bacterium in urine samples or swabs from the genital area.
- Exclusion of Other STIs: Because Mgen symptoms overlap with those of other infections, doctors will often test for other STIs, such as chlamydia or gonorrhea, at the same time.
If you suspect that you might have Mycoplasma genitalium, it’s important to get tested early. Left untreated, Mgen can lead to serious complications, including pelvic inflammatory disease (PID) in women and infertility in both men and women.
4. Mycoplasma Genitalium Treatment Options
Once diagnosed, treating Mycoplasma genitalium is essential to prevent the spread of the infection and to avoid long-term health complications. However, treating Mgen isn’t as straightforward as treating other bacterial infections due to the bacterium’s growing resistance to antibiotics.
Common Treatments:
- Antibiotics: The typical treatment for Mycoplasma genitalium involves a course of antibiotics. However, unlike chlamydia or gonorrhea, Mgen has shown resistance to several commonly used antibiotics, such as azithromycin. Doctors may prescribe moxifloxacin, a more potent antibiotic, if resistance is suspected.
- Follow-Up Testing: After completing the course of antibiotics, it’s important to return for follow-up testing to ensure the infection has been cleared. The persistence of Mgen can lead to complications, and without treatment, it may spread to sexual partners.
- Partner Notification: If you are diagnosed with Mgen, it’s essential to inform any sexual partners so they can get tested and treated as well. This helps to prevent re-infection and stops the spread of the bacterium.
Treatment Challenges:
Due to its antibiotic resistance, treating Mycoplasma genitalium can be challenging. Researchers are continually working on developing new treatment strategies, but for now, it’s crucial to follow your doctor’s advice carefully and complete the entire course of antibiotics.
If you are undergoing treatment for mycoplasma genitalium, it’s also recommended to abstain from sexual activity until the infection is fully cleared to avoid passing it to others.
5. Preventing Mycoplasma Genitalium Infections
While it’s important to know how to recognise and treat Mycoplasma genitalium, prevention is always the best strategy when it comes to STIs. Since Mgen spreads primarily through sexual contact, practicing safe sex is essential.
Prevention Tips:
- Use Protection: Consistent and correct use of condoms during sexual activity can greatly reduce the risk of contracting or transmitting Mgen. While condoms aren’t 100% effective, they offer significant protection.
- Get Regular Screenings: Regular STI screenings are crucial, especially if you have multiple sexual partners or engage in unprotected sex. Early detection allows for prompt treatment and reduces the risk of complications.
- Communicate with Sexual Partners: Open communication with sexual partners about STI testing and protection is vital. Make sure both you and your partner(s) are tested before engaging in sexual activity.
- Limit Sexual Partners: Reducing the number of sexual partners can also lower your risk of contracting Mgen or other STIs.
Conclusion
Mycoplasma genitalium is a hidden STI that often goes undetected due to its overlapping symptoms with other infections. However, its potential to cause long-term health issues makes it a condition that requires attention and care. If you’re experiencing any Mgen symptoms or have had unprotected sex, it’s important to get tested as soon as possible. With early diagnosis and appropriate mycoplasma genitalium treatment, you can protect yourself and your sexual partners from this stealthy bacterium.
Make sure to stay informed, practice safe sex, and take steps to ensure you and your partners are STI-free. To learn more or to schedule a consultation, visit MD.co.uk today.